Specialty Dental Services in Pasco, WA
Why race across town to dentists you don’t know? We provide comprehensive, specialized dental care in one familiar place.

A gum graft (also known as a gingival graft or periodontal plastic surgery), is a collective name for surgical periodontal procedures that aim to cover an exposed tooth root surface with grafted oral tissue.
Exposed tooth roots are usually the result of gingival recession due to periodontal disease. There are other common causes, including overly aggressive brushing and trauma.
Here are some of the most common types of gum grafting:
- Free gingival graft – This procedure is often used to thicken gum tissue. A layer of tissue is removed from the palate and relocated to the area affected by gum recession. Both sites will quickly heal without permanent damage.
- Subepithelial connective tissue graft – This procedure is commonly used to cover exposed roots. Tissue is removed fairly painlessly from the outer layer of the palate and relocated to the site of gum recession.
- Acellular dermal matrix allograft – This procedure uses medically processed, donated human tissue as a tissue source for the graft. The advantage of this is procedure is that there is no need for a donor site from the patient’s palate (and thus, less pain).
Reasons for gum grafting
Gum grafting is a common periodontal procedure. Though the name might sound frightening, the procedure is commonly performed with excellent results.
Here are some of the major benefits associated with gum grafting:
- Reduced sensitivity – When the tooth root becomes exposed, eating or drinking hot or cold foods can cause extreme sensitivity to the teeth. Gum grafting surgery permanently covers the exposed root, helps reduce discomfort, and restores the good health of the gums.
- Improved appearance – Periodontal disease is characterized by gum recession and inflammation. Gum recession and root exposure can make the teeth look longer than normal and the smile to appear “toothy.” Gum grafting can make the teeth look shorter, more symmetrical and generally more pleasing to look at. In addition, adjacent tissue can be enhanced and augmented during the procedure for aesthetic purposes.
- Improved gum health – Periodontal disease can progress and destroy gum tissue very rapidly. If left untreated, a large amount of gum tissue can be lost in a short period of time. Gum grafting can help halt tissue and bone loss; preventing further problems and protecting exposed roots from further decay.
What does gum grafting treatment involve?
Once the need for gum grafting surgery has been determined, there are several treatments the dentist will want perform before gum grafting takes place. First, the teeth must be thoroughly cleaned supra and subgingivally to remove calculus (tartar) and bacteria. The dentist can also provide literature, advice and educational tools to increase the effectiveness of homecare and help reduce the susceptibility of periodontal disease in the future.
The gum grafting procedure is usually performed under local anesthetic. The exact procedure will depend much on whether tissue is coming from the patient’s palate or a tissue bank.
Initially, small incisions will be made at the recipient site to create a small pocket to accommodate the graft. Then a split thickness incision is made and the connective tissue graft is inserted into the space between the two sections of tissue. The graft is usually slightly larger than the recession area, so some excess will be apparent.
Sutures are often placed to further stabilize the graft and to prevent any shifting from the designated site. Surgical material is used to protect the surgical area during the first week of healing. Uniformity and healing of the gums will be achieved in approximately six weeks.
In the past, if you had a tooth with a diseased nerve, you’d probably lose that tooth. Now, with “root canal therapy,” your tooth can be saved. When a tooth is cracked or has a deep cavity, bacteria can enter the pulp tissue and germs can cause an infection inside the tooth. If left untreated, an abscess may form. If the infected tissue is not removed, pain and swelling can result. This can injure your jawbones and be harmful to your overall health.
Root canal therapy involves one to three visits. During treatment, your general dentist or endodontist removes the affected tissue. Next, the interior of the tooth will be cleaned and sealed. Finally, the tooth is filled with a dental composite. If your tooth has extensive decay, your dentist may suggest placing a crown to strengthen and protect the tooth from breaking. As long as you continue to care for your teeth and gums with regular brushing, flossing, and checkups, your restored tooth can last a lifetime.
What is a root canal procedure?
Tooth decay can progress down into the pulp. When this happens, the pulp can become infected. Infection of the pulp can be very painful and can also deteriorate into an abscessed tooth when infection and swelling develops in the tissues around or beneath the tooth. When the pulp becomes infected or the tooth becomes abscessed, it is necessary to perform a root canal.
Why do I feel pain?
When the pulp becomes infected due to a deep cavity or fracture, bacteria can seep in. When there has been an injury due to trauma, the pulp can die. Damaged or dead pulp causes increased blood flow, pressure, and cellular activity. Pain in the tooth is commonly felt when biting down or chewing, and eating or drinking hot and/or cold foods and beverages.
Why do I need root canal therapy?
The tooth will not heal by itself. Without treatment, the infection will spread. The bone around the tooth will begin to degenerate, and the tooth may fall out. Pain usually worsens until one is forced to seek emergency dental attention. The only alternative is extraction of the tooth, which can cause the surrounding teeth to shift, resulting in a bad bite. Though an extraction is cheaper, the space left behind will require an implant or a bridge, which can be more expensive than root canal therapy. If you have the choice, it’s always best to keep your original teeth.
What are the risks and complications with root canal therapy?
More than 95 percent of root canal therapies are successful. However, sometimes a case needs to be redone due to diseased canal offshoots that went undetected, or the fracturing of the canal filling. More commonly, a root canal therapy will fail altogether, marked by the return of pain.
What happens after root canal therapy?
Once root canal therapy is completed, the endodontist will refer the patient back to our office for the permanent restoration on the tooth. A temporary filling was placed immediately following the root canal therapy and will need to be replaced with a permanent filling or crown and build up. A crown will be necessary on all posterior teeth to properly protect the root canal- treated tooth from fracturing. Front teeth can typically be restored with a filling, however a crown may be necessary in some cases. Your dentist will determine the best choice for your individual needs.
How long will the restored tooth last?
Your restored tooth could last a lifetime, if you continue to care for your teeth and gums. However, regular checkups are necessary. As long as the root(s) of a treated tooth are nourished by the tissues around it, your tooth will remain healthy.
How does root canal therapy save my tooth?
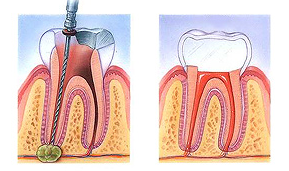
- An opening is made through the crown of the tooth into the pulp chamber.
- The pulp is removed, and the root canals are cleaned, enlarged and shaped.
- Medications may be put in the pulp chamber and root canal(s) to help get rid of germs and prevent infection.
- A temporary filling will be placed in the crown opening to protect the tooth between dental visits. Your dentist may leave the tooth open for a few days to drain. You might also be given medicine to help control infection that may have spread beyond the tooth.
- The temporary filling is removed and the pulp chamber and root canal(s) are cleaned and filled.
- In the final step, a gold or porcelain crown is usually placed over the tooth.

In rare cases, root canal therapy fails to work as expected. The treated tooth might not heal properly or a patient might experience post-surgical complications that jeopardize the tooth. Root canal retreatment involves the removal of the previous crown and packing material, the cleansing of the root canals, and the re-packing and re-crowning of the tooth. In short, root canal retreatment is almost identical to the original procedure, aside from the structural removal. The success rate for a root canal retreatment runs at around 75%.
Root canal treatments and retreatments are a better alternative than extraction for most individuals. If a tooth has good bone support, a solid surface and healthy gums beneath it, it stands a good chance of being saved. Opting for root canal retreatment can be far less expensive than the alternatives. Dental implants, extensive bridgework and the creation of aesthetically pleasing prosthetic teeth cost far more than working with the natural tooth. They also require maintenance and feel less natural than a “real” tooth.
Why is root canal retreatment required?
Though the prospect of more endodontic surgery might not be pleasant, root canal retreatment is fairly simple. In general, the whole treatment can be completed in 1-3 visits.
There are a number of reasons why root canal therapy unexpectedly fails, including:
- Cracked crown leaking filling material
- Curved or narrow canals not treated during the original procedure
- Delay in the placement of restorative devices following the procedure
- New decay to the tooth
- New fracture in the treated tooth
- Saliva entering the restorative structure
- Undetected complex canal structures
What does root canal retreatment involve?
On the day of the retreatment procedure a local anesthetic will be administered, unless another type of anesthetic has been selected. The affected tooth is isolated with a rubber dam. The dam protects the tooth during treatment from bacteria and saliva. The amount the dentist can do within a single appointment will much depend on the amount of inflammation present, and the complexity of the treatment.
The first step in a root canal retreatment is to gain access to the inner tooth. If a crown and post have been placed, these will be removed.
Next, filling material and obstructions that block the root canals will be removed. This removal is conducted using an ultrasonic handpiece. The advantage of using this tool is that any unwanted material is vibrated loose. Tiny instruments will then be used to clean and reshape the root canals. X-rays may be taken to ensure that the roots are thoroughly clean. If this part of the treatment proves to be complex, medicated packing material will be applied, and the rest of the cleansing procedure will be done at the next visit.
When the dentist is confident that the root canals are completely clean, gutta-percha is used to pack the space. This rubbery material seals the canals to prevent bacterial invasion. Finally, a temporary crown or filling is applied to tooth. At a later date, the color-matched permanent crown will be placed.

The objective of scaling & root planning is to remove etiologic agents which cause inflammation to the gingival (gum) tissue and surrounding bone. Common etiologic agents removed by this conventional periodontal therapy include dental plaque and tartar (calculus).
These non-surgical procedures which completely cleanse the periodontium, work very effectively for individuals suffering from gingivitis (mild gum inflammation) and moderate/severe periodontal disease.
Reasons for scaling and root planing
Scaling and root planning can be used both as a preventative measure and as a stand-alone treatment. These procedures are performed as a preventative measure for a periodontitis sufferer.
Here are some reasons why these dental procedures may be necessary:
- Disease prevention – The oral bacteria which cause periodontal infections can travel via the bloodstream to other parts of the body. Research has shown that lung infections and heart disease have been linked to periodontal bacteria. Scaling and root planing remove bacteria and halts periodontal disease from progressing, thus preventing the bacteria from traveling to other parts of the body.
- Tooth protection – When gum pockets exceed 3mm in depth, there is a greater risk of periodontal disease. As pockets deepen, they tend to house more colonies of dangerous bacteria. Eventually, a chronic inflammatory response by the body begins to destroy gingival and bone tissue which may lead to tooth loss. Periodontal disease is the number one cause of tooth loss in the developed world.
- Aesthetic effects – Scaling and root planing help remove tartar and plaque from the teeth and below the gumline. As an added bonus, if superficial stains are present on the teeth, they will be removed in the process of the scaling and root planning procedure.
- Better breath – One of the most common signs of periodontal disease is halitosis (bad breath). Food particles and bacteria can cause a persistent bad odor in the oral cavity which is alleviated with cleaning procedures such as scaling and root planing.
What do scaling and root planing treatments involve?
Scaling and root planing treatments are only performed after a thorough examination of the mouth. The dentist will take X-rays, conduct visual examinations and make a diagnosis before recommending or beginning these procedures.
Depending on the current condition of the gums, the amount of calculus (tartar) present, the depth of the pockets and the progression of the periodontitis, local anesthetic may be used.
Scaling – This procedure is usually performed with special dental instruments and may include an ultrasonic scaling tool. The scaling tool removes calculus and plaque from the surface of the crown and root surfaces. In many cases, the scaling tool includes an irrigation process that can also be used to deliver an antimicrobial agent below the gums that can help reduce oral bacteria.
Root Planing – This procedure is a specific treatment which serves to remove cementum and surface dentin that is embedded with unwanted microorganisms, toxins and tartar. The root of the tooth is literally smoothed in order to promote good healing. Having clean, smooth root surfaces helps bacteria from easily colonizing in future.
Following these deep cleaning procedures, the gum pockets may be treated with antibiotics. This will soothe irritation and help the gum tissues to heal quickly.
During the next appointment, the dentist or hygienist will thoroughly examine the gums again to see how well the pockets have healed. If the gum pockets still measure more than 3mm in depth, additional and more intensive treatments may be recommended.
A significant number of Americans do not visit the dentist for regular checkups because they are too fearful or suffer from dental anxiety. Sedation dentistry offers an excellent way to provide a safe, anxiety-free, dental experience to those who are afraid of the dentist.
Sedation dentistry is often mistakenly thought to induce sleep. In fact, most sedatives allow the patient to stay awake during the procedure. Sleepiness is a side effect of some medications, but nitrous oxide, oral conscious sedation and IV sedation only work to calm anxiety throughout the dental visit.
Sedation dentistry is popular because most sedatives can be taken by mouth, meaning no injections, no anxiety and no pain. Some sedatives work so effectively that even the smells and details of the procedure cannot be recalled afterwards. Safety and compliance are two important aspects of treatments, so sedation dentistry offers both the individual and the dentist the best alternative.
Whatever the form of sedative, it is essential to be accompanied by a caregiver. Sometimes, sedatives are provided the night before the dental visit, which means that driving to or from the appointment is not advisable.
Here are some advantages associated with sedation dentistry:
- Anxiety is alleviated.
- Few side effects.
- More can be accomplished during each visit.
- No needles.
- No pain.
- Perfectly safe.
- Procedures seem to take less time.
What kinds of sedatives are available?
The most popular types of dental sedatives are nitrous oxide and oral conscious sedation. Different levels of sedation (mild, moderate and deep) can be utilized depending on individual needs. Before administering any sedative, the dentist must analyze the full medical history of the patient, as well as taking note of any current medications.
Nitrous Oxide
Nitrous oxide, or “laughing gas,” is used as a mild sedative. It is delivered through a nose hood, and is administered throughout the entire procedure. Nitrous oxide elevates the general mood and can evoke a general sense of well-being. Most importantly, it relieves anxiety and reduces pain during the procedure. In addition, some tingling and numbness may be felt. There are few side effects associated with nitrous oxide, and it has been safely used in dentistry for many years.
Oral Conscious Sedation
Oral conscious sedation is an excellent choice for people who fear needles. Oral medication is provided prior to treatment in order to induce a moderate state of sedation. Though oral sedatives do not cause sleep, they usually dull the senses. This means that most patients cannot remember the pain, smells or noises associated with the procedure. Usually, a dose of medication is taken prior to the appointment, and then topped up during the procedure as required.
What types of drugs are used in oral conscious sedation?
Most of the drugs used in sedation dentistry are classified as benzodiazepines. Benzodiazepines reduce anxiety, muscle spasms, insomnia and seizures. Each medication has a different half-life, meaning that the effects last for varying amounts of time. The estimated length of the procedure determines which type of drug is going to be most effective.
Here are some of the most common drugs used in oral conscious sedation:
Valium® – This sedative has amnesic properties and a long half-life. It is usually used for time-consuming, complex procedures.
Halcion® – Usually used to treat insomnia, Halcion is an effective sedative with amnesic properties. A short half-life makes this sedative useful for shorter procedures.
Ativan® – This sedative is best known for reducing anxiety. It has amnesic properties and a medium half-life. Ativan is typically used for treatments shorter than two hours.
Versed® – This sedative has the shortest half-life and is therefore less commonly used. It alleviates anxiety in much the same way as nitrous oxide, and is used for visits that will take less than 30 minutes.
